New vaccine holds great promise for fighting deadly brain cancer in humans and dogs

In a first-in-human clinical trial involving 4 adult patients in Florida, USA, an mRNA cancer vaccine was able to quickly reprogram the immune system to attack glioblastoma, the most aggressive and deadly brain tumor..
The published results also reflect previous work with 10 dogs suffering from naturally occurring brain tumors whose owners approved their participation because they had no other treatment options, as well as results from preclinical mouse models. This breakthrough will now be tested in a Phase 1 pediatric brain cancer clinical trial.
The opening represents potential new way to recruit the immune system to fight notoriously treatment-resistant cancers using an iteration of mRNA and lipid nanoparticle technology similar to COVID-19 vaccines, but with two key differences: the use of a patient’s own tumor cells to create a personalized vaccine and a complex mechanism, a newly developed delivery system within the vaccine.
“Instead of introducing individual particles, we introduce groups of particles that wrap around each other like an onionlike a bag full of onions,” the authors explain new vaccinewhich, like other immunotherapies attempts to “teach” the immune system that the tumor is foreign. “And the reason we did this in the context of cancer is because these clusters alert the immune system much deeper than individual particles.”
PROGRESS IN LESS THAN TWO DAYS
Among the most impressive discoveries was the speed with which a new method, administered intravenously, caused a violent reaction immune system to reject the tumor.
“In less than 48 hours, we were able to see how these tumors went from what we call “cold” (immune cold, very few immune cells, very suppressed immune response) to “hot” and a very active immune response. “This was very surprising given how quickly it happened, and it tells us that we were able to activate the initial part of the immune system against these cancers very quickly, and this is critical to unlocking the downstream effects of the immune response.” “, the researchers note.
He Glioblastoma is one of the most terrible diagnoses. with an average survival of about 15 months. The current standard of treatment includes surgery, radiation therapy, and some combination of chemotherapy.
The new publication is the culmination of promising translation results throughout seven years of study, starting with preclinical mouse models and then clinical trials on 10 dogs that spontaneously developed terminal brain cancer and had no other treatment options. “Dogs provide a natural model for malignant glioma because It is the only species that develops spontaneous brain tumors with any frequency.. Gliomas in dogs are always terminal,” they say.
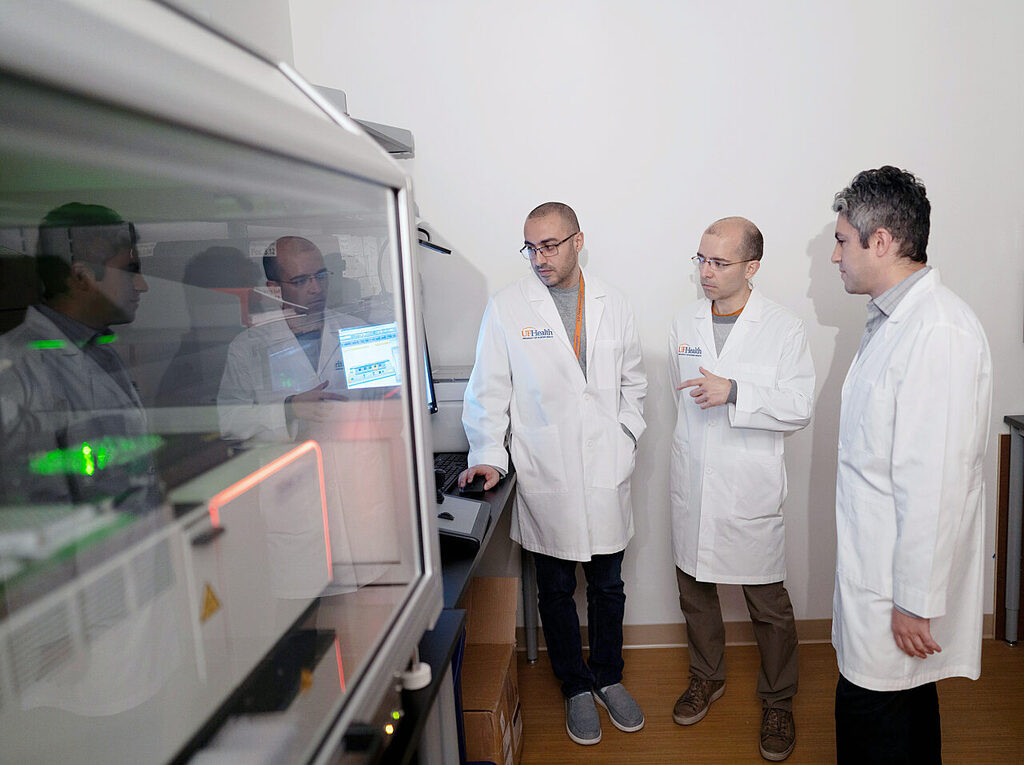
After treating dogs that spontaneously developed brain cancer with personalized mRNA vaccines, the team moved the study to a small clinical trial to ensure safety and feasibility of testing before moving on to a larger study.
In a group of four patients, genetic material called RNA was extracted from each surgically removed tumor, then messenger RNA, or mRNA (the blueprint for what’s inside every cell, including tumor cells), was amplified and wrapped in a new design-tech packaging biocompatible lipid nanoparticles, which make it possible to give tumor cells the appearance of a dangerous virus when they re-enter the bloodstream and trigger a response from the immune system. The vaccine has been tailored to each patient to make the most of their unique immune system.
“Demonstrating that creating an mRNA vaccine against cancer in this way produces similar strong responses in mice, dogs that spontaneously developed cancer, and patients with brain cancer. This is a really important find.And, because we often don’t know how well preclinical studies work. Animal studies will lead to similar reactions in patients,” they point out. “And while mRNA vaccines and treatments are certainly a hot topic post-COVID, this a new and unique method of delivering mRNA generate the truly meaningful and rapid immune responses that we see in animals and humans.”
Although the study was too early to assess the clinical effects of the vaccine, patients lived without disease longer than expected or survived longer than expected.
The 10 dogs lived an average of 139 days, while the average survival rate for dogs with this disease was 30 to 60 days.
WHAT’S NEXT?
The next step will be an expanded Phase I clinical trial that will enroll up to 24 adults and children to test the findings. It is expected that after confirmation of the optimal and safe dose, 25 children will participate in the second stage.
For the new clinical trial, they will collaborate with a multi-institution consortium. send immunotherapy treatments to children’s hospitals across the United States.. They will do this by obtaining an individual patient’s tumor, making a personalized vaccine, and sending it back to the patient’s medical team.
Despite the promising results, the authors believe that One limitation is the ongoing uncertainty about how best to harness the immune system while minimizing the likelihood of adverse side effects..
“We hope this can be new paradigm in how we treat patients, a new technology platform that allows modulation of the immune system. Additionally, this could now interact with other immunotherapies and possibly open up these immunotherapies. In this article We’re showing that you can actually have synergy with other immunotherapies.so perhaps we can now use a combination approach to immunotherapy.”