Revolutionary vaccine teaches the immune system to fight HIV step by step
The sequential vaccination strategy to obtain an effective vaccine against the HIV virus is yielding its first results. C. The research team publishes four papers simultaneously (two in Science, one in Immunology Science, and one in Translational Medicine Science). … including advances in developing a class of HIV vaccines that could provide broad protection against the virus.
“The development of a preventive vaccine against HIV infection is one of the most important unresolved issues in HIV research, and unfortunately it has been a history of failure so far,” said José Alcami, director of the Department of AIDS Immunopathology, ABC Salud of Carlos III. Institute of Health.
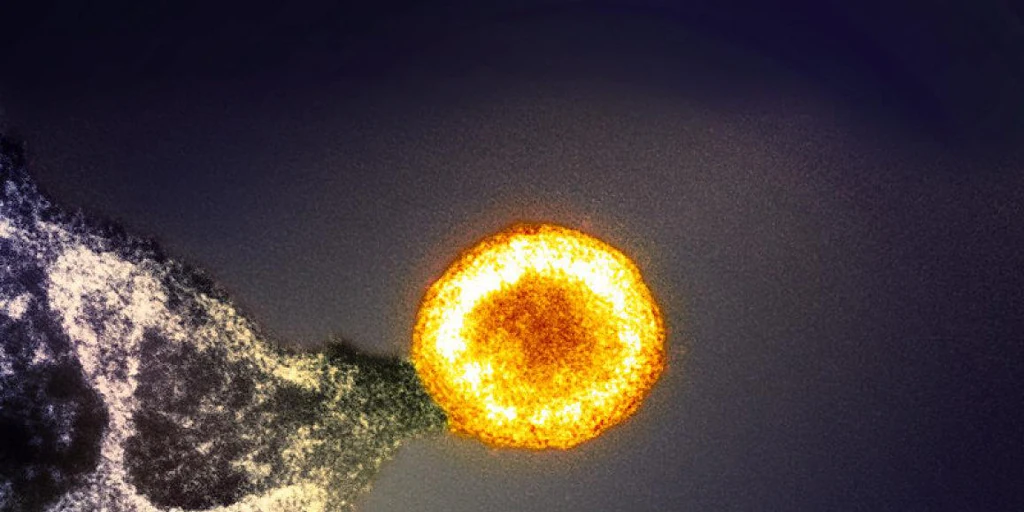
As the HIV epidemic enters its fifth decade, scientists are pouring time and resources into developing vaccines against the virus, although with limited success. One proposed solution involves a process called germline targeting, in which a series of immune system-targeted proteins (immunogens) are used to guide and “court” young B cells as they mature in areas called germinal centers. The goal is to induce cells to produce broadly neutralizing HIV antibodies that can recognize many types of HIV and block it from entering healthy cells.
The goal of a prophylactic vaccine is to induce the production of neutralizing antibodies that block viral infection. This, as Alkami notes, “This is achieved through antigens, which include surface proteins of the virus that interact with cellular receptors.. However, the structure of the HIV envelope makes this difficult because it is designed to conceal interaction domains and is highly glycosylated, forming a “glycan shield.”
Over the past decade, vulnerable regions of the HIV envelope that are accessible to antibodies have been identified. However, he continues, “these antibodies are rare and must have a specific structure, such as an extension of the HCDR3 domain, to overcome barriers. In addition, the antibodies that are initially formed have low affinity and require a long maturation process.
However, Two key lessons emerged from these difficulties.And, emphasizes: first, “an effective HIV vaccine must be based on selective envelope structures that immunogenically expose vulnerable areas of the virus. In addition, sequential vaccinations with slightly different prototypes are necessary to induce antibody maturation and achieve a potent response.
B lymphocytes
Four articles published in the Science group create immunogens/vaccines aimed at activating B lymphocytes – cells of the immune system capable of producing antibodies with these characteristics and specifically directed against two regions of the viral envelope. : CD4 binding domain and V3 region.
Specifically, in papers published in the journal Science, William Schiff’s group at the Scripps Institute created a protein (N332-GT5) that specifically activates germline B lymphocytes in primates, the precursors of BG18-type neutralizing antibodies (potent neutralizing antibodies). . The team showed that their approach successfully stimulated and increased the number of B cells secreting BG18 precursors (a broadly neutralizing antibody against HIV) in a group of eight rhesus monkeys.
In another work published in the journal Science, another group from the Scripps Institute used mRNA to prime B cells with the immunogen N332-GT5 administered via lipid nanoparticles to humanized mice. This method activated and increased B cells, reducing unwanted effects..
The journal Science Translational Medicine published a new nanoparticle immunogen to enhance HIV vaccines, and the journal Science Immunology showed that mRNA encapsulated in lipid nanoparticles can be used to deliver the immunogen. This prompted B cells to diversify and produce effective antibodies against HIV in mice.
The goal of a prophylactic vaccine is to induce the production of neutralizing antibodies that block viral infection.
This strategy is already known and has been used before, says Julia Blanco, head of the virology and cellular immunology group at the IrsiCaixa AIDS Research Institute, in an interview with Science Media Center. “The HIV envelope protein has different regions that are recognized by neutralizing antibodies. For a specific region (CD4 binding site), this strategy has already been used and has even reached human studies. Now we have a second area (loop base V3) that can also be used in a similar way. By combining both strategies, a greater number and variety of these neutralizing antibodies could be generated. (which would make the potential vaccine more effective).
Blanco elaborates that because of the “difficulty of creating neutralizing antibodies against HIV, the authors direct the immune system to produce a specific type of neutralizing antibody with different immunogens: first simpler ones (so that they can be better recognized), and then more complex and related ones.” to the original HIV envelope protein. The studies are technically excellent and deeply analyze the evolution of antibodies that are generated sequentially.
Amelia Escolano, whose laboratory at the Center for Vaccines and Immunotherapy of the Wistar Institute (USA) has been working in this field for many years, explains to ABC Salud that, unlike traditional vaccination systems, in which the same immunogen is administered repeatedly, several times,What is done is to inject different versions of the immunogen one after another to direct the antibody response to the epitopes of interest and cause those antibodies to mature so that they become capable of neutralizing HIV.”
So, adds the Wistar researcher, “we start by injecting a highly modified version of the HIV envelope protein, and later, instead of injecting it again, we inject another slightly less modified version that is more similar to the natural HIV protein.” envelope. “Successively fewer and fewer modified envelope proteins are introduced until finally one that is unmodified, the wild type, is introduced.”
For the ISCIII researcher, although in very restrictive preclinical models, these papers represent proof of concept. “Phase I trials in volunteers will confirm whether data from animal models can be extrapolated to humans, which has not always been observed.”
Blanco believes the main limitation is that the studies published in the journal Science were conducted in animals and cannot be quantitatively transferred to humans.
Moreover, he adds, research clearly shows us the difficulty of creating an HIV vaccine. “Sequential vaccination can be an excellent strategy, but it may require excessive amounts of immunogens, making it difficult to translate this strategy into a product that reaches the population most in need. There’s a lot of work ahead“
