technological revolution in diabetes treatment

In recent years, the development of new drugs, improvements in microprocessors and sensors, and access to software free have significantly improved diabetes treatment and adapted it to the characteristics of each patient. Below we will look at the main milestones of this revolution.
The first pumps and glucometers
The history of technological control of diabetes began in the mid-1960s. It was then that the first insulin pump was developed for patients with type 1, who depend on external supply of this hormone.
A little later, in the seventies, the first glucometer (glucometer) was designed, allowing for its direct recording. Previously, the only way to do this was with test strips that changed color when they came into contact with glucose present in the urine. However, this was an imprecise technique because it indicated an approximate range and depended on the level of fluid intake.
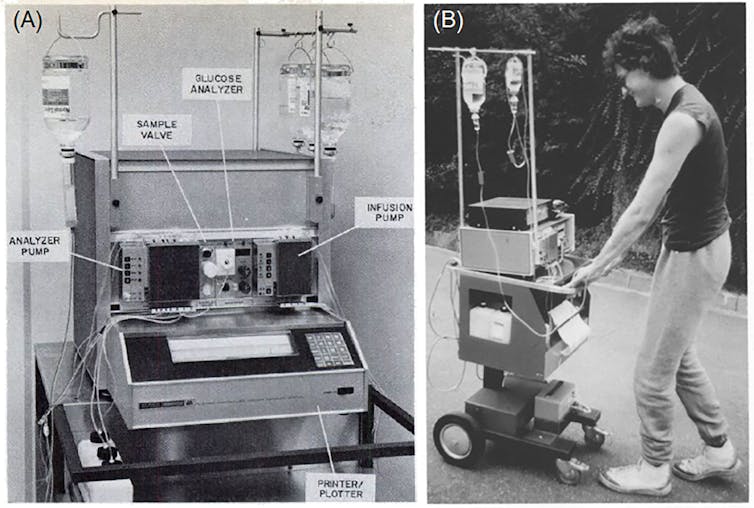
Frontiers / Closed-loop insulin delivery systems: directions of the past, present and future
These instruments from the sixties and seventies were useful in hospitals, but given their size and price, they were not available to patients.
In recent decades, developments in microelectronics have enabled devices to become miniaturized, offering detailed and personalized glucose information in real time. This allows you to make more accurate decisions.
Algorithms for health
Continuous monitors attached to the skin have now largely replaced blood glucose meters. They collect glucose data every few minutes, offering automatic alerts and suggestions based on patterns detected.
These are systems that can predict imminent changes in these levels and, in some cases, interact with insulin pumps to automatically adjust delivery. This intelligent interaction is known as an “artificial pancreas” and has proven to be a very powerful tool in the fight against type 1 diabetes.

Source: author’s preparation.
Currently, patients have blood glucose monitors and insulin pumps that are attached to their abdomen. The data is collected and transmitted via Bluetooth to the mobile phone, which processes it using advanced algorithms and sends the appropriate commands to the pump.
Type 2 diabetes, the most common form of the disease, has also benefited from these skin-attached monitors with apps that can closely monitor glucose levels and activity patterns.
Treatment tailored to the patient
Moreover, the movement software free, open source, allows you to improve treatment methods. While the level of configuration available in these tools can be overwhelming, they allow you to customize everything from meal timing to insulin delivery for specific situations such as exercise or sleep.
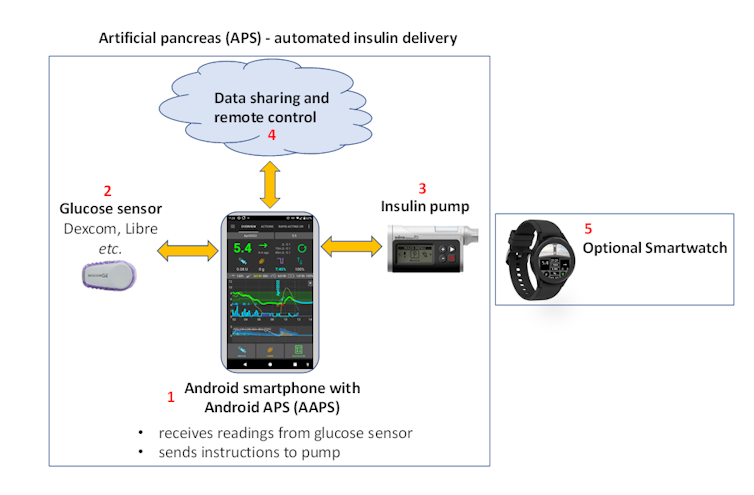
AndroidAPS Community
For many people with type 1 diabetes, these options represent a previously unattainable level of freedom and control. However, it should also be noted that excessive personalization without the supervision of a healthcare professional can be risky. The decision about any key adjustments should always be made in consultation with an endocrinologist.
This technology is not only microelectronics: it also includes pharmaceutical innovations such as drugs whose active ingredient is semaglutide: Wegovy, Ozempic and Mounjaro. They were originally developed to treat type 2 diabetes, but are widely used for weight loss. The demand for this type of medicine has exceeded all expectations, and there are even black supply markets.
In any case, it is worth remembering that, regardless of technology, good eating habits have always been a fundamental element of diabetes control. Any dietary change should be made under the guidance of a healthcare professional, and this is especially important for patients with metabolic diseases such as type 1 or type 2 diabetes.
Barriers and future opportunities
Despite the innovations described, there are barriers that prevent innovation from reaching all patients. On the one hand, the cost of new devices and drugs remains a significant constraint, especially in countries with more fragile healthcare systems or without sufficient coverage.
The future promises new technological advances in the fight against diabetes, and it is possible that we will soon be able to use artificial intelligence. However, neither a fad diet, nor the latest technology, nor the drugs used by celebrities can be adopted as a magic solution.
In any case, it is not expected that patients with diabetes will no longer require the supervision of health care providers. They are the ones who can really help you optimally combine the right medications, technology, proper nutrition and exercise.
