AI helps Chuvi radiologists speed up prostate cancer diagnosis
The diagnosis of prostate cancer is changing. Once high levels of PSA, the prostate-specific antigen test, raise a red flag, the test is no longer a direct biopsy and a less invasive method should be chosen first: magnetic resonance imaging. Thus, the number of these studies is growing. The head of the Radiological Diagnostic Service, Dr. Milagros Otero, estimates there are about 25 a week. To speed up the preparation of reports and improve diagnostic accuracy, until the end of the year, the University Hospital Complex Vigo (Chuvi) will use artificial intelligence (AI) to generate preliminary reports, which must then be checked by a radiologist.
To do this, they will work with the Valencian company Quirim. Adhering to all privacy and confidentiality requirements, the patient’s MRI images are uploaded to this cloud platform where an algorithm analyzes the images and returns them with a preliminary report detailing the Clinically Significant Cancer Risk Score -PI-RADS- level and lesion areas drawn.
“It helps significantly with diagnosis because it already gives you a preliminary report and maybe detects things you don’t see or reassures you that you see an injury,” Dr. Otero explains and summarizes: it can reduce time and increase reliability.
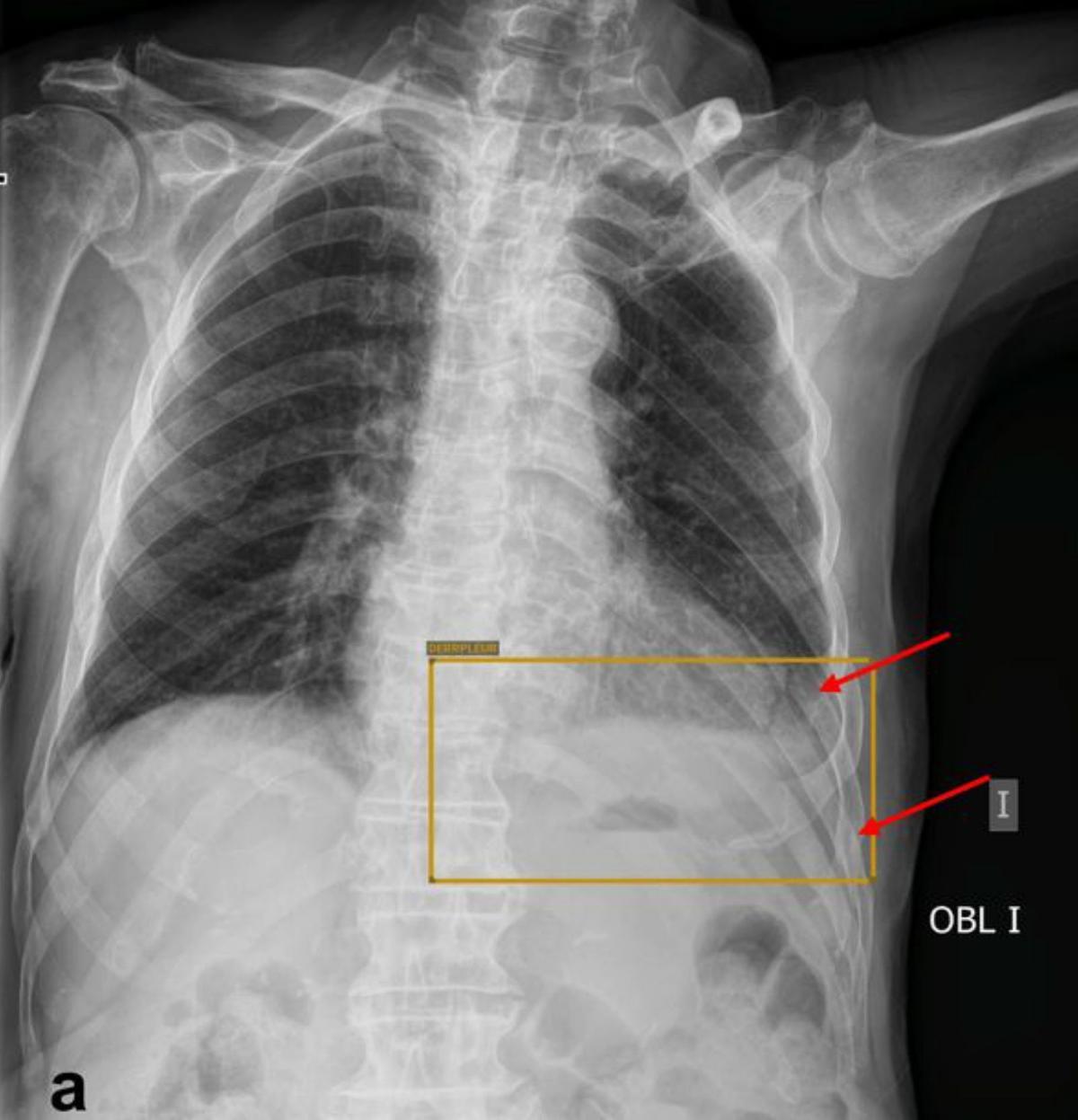
Image of AI notifying family doctors and emergency physicians when a fracture is detected / Fdv
The President of the Spanish Society of Medical Radiology also says that algorithms are now being developed for all pathologies. They hope that the next area where AI will generate preliminary reports will be breast cancer. “They are the most advanced because they are also the most common tumors,” he notes.
AI is permeating virtually every area of healthcare, from resource management processes to early detection or treatment planning.
The radiology service, followed by the cardiology service, is currently the most widely represented.
AI helps with numbers in primary and urgent care
Improvements and reliability of imaging techniques are leading to an increase in the number of queries, and radiologists are unable to report all of them. For example, more than 500 chest and musculoskeletal radiographs are performed daily in primary care settings. “This is impossible to report,” emphasizes Dr. Otero. Radiologists do this with a quarter of them. In cases where there is doubt.
If not, then the family doctor sees her. For months now, primary care physicians have been using artificial intelligence to detect abnormalities on chest X-rays—pneumonia, pleural effusion, lung nodules…—and musculoskeletal abnormalities in patients over 18 years of age. In the latter case, AI is more sensitive for fractures than for degenerative diseases. Therefore, last week they decided to install this tool also at the Álvaro Cunqueiro Emergency Service, where the majority arrive. The technology identifies the abnormality and comments whether it is positive for alveolar fracture or consolidation.
Subscribe to continue reading
