BRCA1 and BRCA2 mutations in metastatic prostate cancer lead to worse prognosis
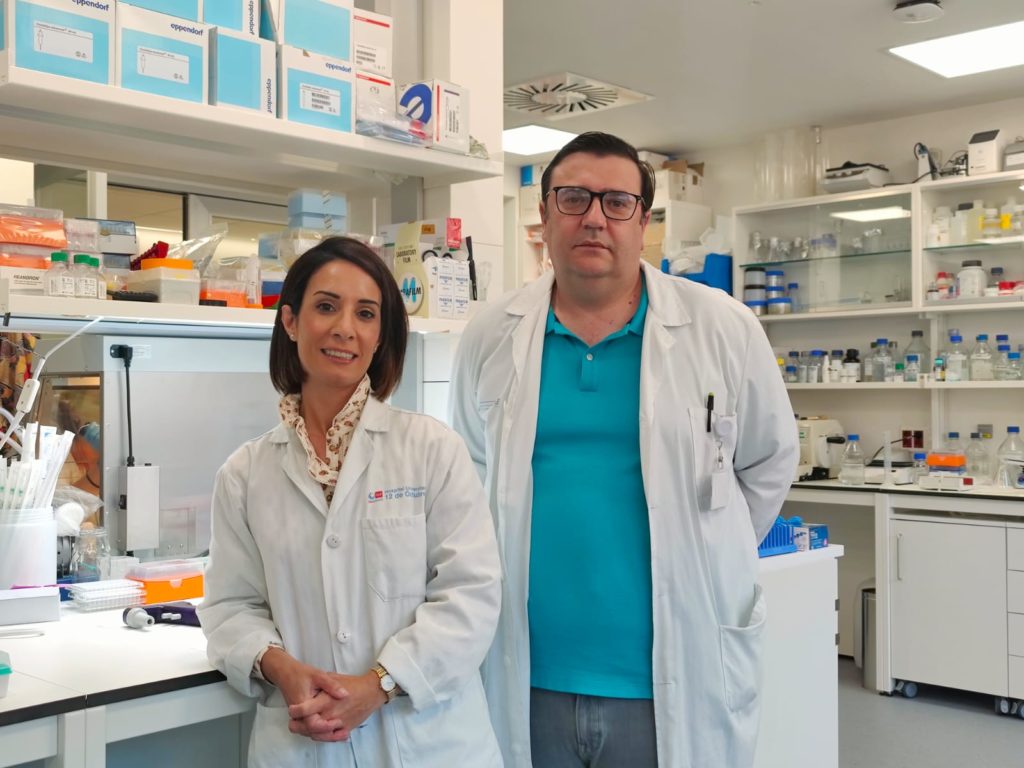
Researchers from the 12 October Hospital in Madrid took part in a study that demonstrated the aggressiveness of a type of prostate cancer associated with mutations in the BRCA1 and BRCA2 genes, for which there is a therapeutic alternative based on the use of PARP inhibitors. .
The results of the study were published in the scientific journal Annals of Oncology. Although Germline BRCA mutations are associated with adverse outcomes in prostate cancerHowever, understanding of somatic/germline alterations in homologous recombination (HRR) genes and treatment outcomes in metastatic castration-resistant prostate cancer (mCRPC) has been limited.
In this sense, this study delved into the prevalence and outcomes associated with these changes, especially in BRCA1 and BRCA2, in patients with mCRPC who initiate first-line treatment with androgen receptor signaling inhibitors (ARSi) or taxanes.
“In this study, we sought to explore what the implications of alterations in DNA repair genes in prostate tumors may be for the response to available treatments and prognosis for patients with advanced prostate cancer,” they explain. Elena Castro, senior author and researcher at the October 12 Hospital Research Institute. “
Research method
The researchers combined the data 729 patients with mCRPCderived from four multicenter observational studies that used ARSi or taxanes as first line and had adequate tumor samples.
These patients passed Paired analyzes of normal and tumor DNA through next generation sequencing using a gene panel that included: ATM, BRCA1, BRCA2, BRIP1, CDK12, CHEK2, FANCA, HDAC2, PALB2, RAD51B, and RAD54L. Subsequently, based on the results obtained, individuals were divided into groups depending on the somatic changes in the germline represented in them; with BRCA1/2 mutations, with HRR mutations other than BRCA1/2 (HRR without BRCA), and without HRR changes (HRR without changes). Finally, radiographic progression-free survival (rPFS), progression-free survival 2 (PFS2), and overall survival (OS) were assessed.
Of the total patients, 96 (13.2%) fell into the BRCA mutation subgroup; 127 (17.4 percent) in the non-BRCA HRR group; and 506 (69.4 percent) in the non-HRR group. When comparing data Patients with BRCA had significantly worse outcomes than the other groups, just as they had shorter PFS2 and OS than non-HRR and non-BRCA patients.
“We have observed that patients who have certain changes, especially in the BRC1 or BRC2 genes, whether inherited or acquired by the tumor, benefit less from the conventional treatments we currently have, such as chemotherapy or androgen receptors. The survival rate of these patients is almost half than in patients who do not have these types of changes,” says the specialist.
In conclusion, patients with mCRPC in the BRCA subgroup compared with non-BRCA subgroups have worse outcomes. And he early screening for HRR mutationsespecially BRCA1/2, is important for improving the prognosis of mCRPC patients.
PARP inhibitors
The research team also confirmed that the use Polyadenosine disphosphate ribose polymerase inhibitors (PARPi) provide significant results. and an important clinical benefit for patients with mCRPC with alterations in specific genes directly or indirectly associated with HRR. In this case, the findings suggest that treatment with ARSi in combination with PARPi is the first-line treatment for patients with HRR changes in tumors, especially BRCA1/2may progress faster than with standard treatment for ARSI.
“In recent years, treatments known as PARP inhibitors have been developed that work particularly well in patients with changes in these genes. These treatments have been used for several years in ovarian cancer as well as breast cancer, and since 2020 several studies have been conducted in which proven effectiveness and benefit for prostate cancer“,” says Castro, adding that “it was demonstrated first in more advanced stages, and little by little the research moved into earlier phases.”
You may also like…
