CNIO proposes new treatment for brain metastases using immunotherapy
Researchers from the National Center for Cancer Research (CNIO) propose a new treatment for brain metastases that do not respond or respond poorly to immunotherapy, and provide a biomarker to predict when to use it. Our body has a mechanism for destroying everything that attacks it, be it viruses,…
Researchers from the National Center for Cancer Research (CNIO) propose a new treatment for brain metastases that do not respond or respond poorly to immunotherapy, and provide a biomarker to predict when to use it.
Our body has a mechanism for destroying anything that attacks it, be it viruses, bacteria or cancer cells: the immune system. Cancer multiplies when tumor cells trick this system from being activated against them. Cancer immunotherapy uses drugs to prevent cancer cells from blocking the immune system, but immunotherapy does not always work.
For brain metastases—when a tumor that originates in an organ spreads to the brain—immunotherapy has recently been tried, with mixed results.
“Brain metastases represent a serious clinical problem”explains Manuel Valiente, Head of the Brain Metastasis Group at CNIO and Study Leader which is now publishing its results. “Patients with brain metastases, that is, those who are already experiencing symptoms of metastases, respond poorly to immunotherapy. But it is also increasingly common for patients who have responded well to immunotherapy to relapse, as “this often occurs due to new brain metastases.”adds Valiente, a recipient of a grant from the European Research Council (ERC).
That is, immunotherapy with blocking antibodies does not seem to be the optimal system for brain metastases. A possible reason is the existence of the blood-brain barrier, a type of permeable membrane that filters blood entering the brain and protects it from toxins. But this vascular barrier also makes it difficult for antibodies used in immunotherapy to penetrate. Without antibodies, immunotherapy does not work.
Astrocytes that side with cancer
The CNIO group now proposes a very innovative hypothesis to combat this problem. This was reported in the journal Cancer Discovery of the American Association for Cancer Research.
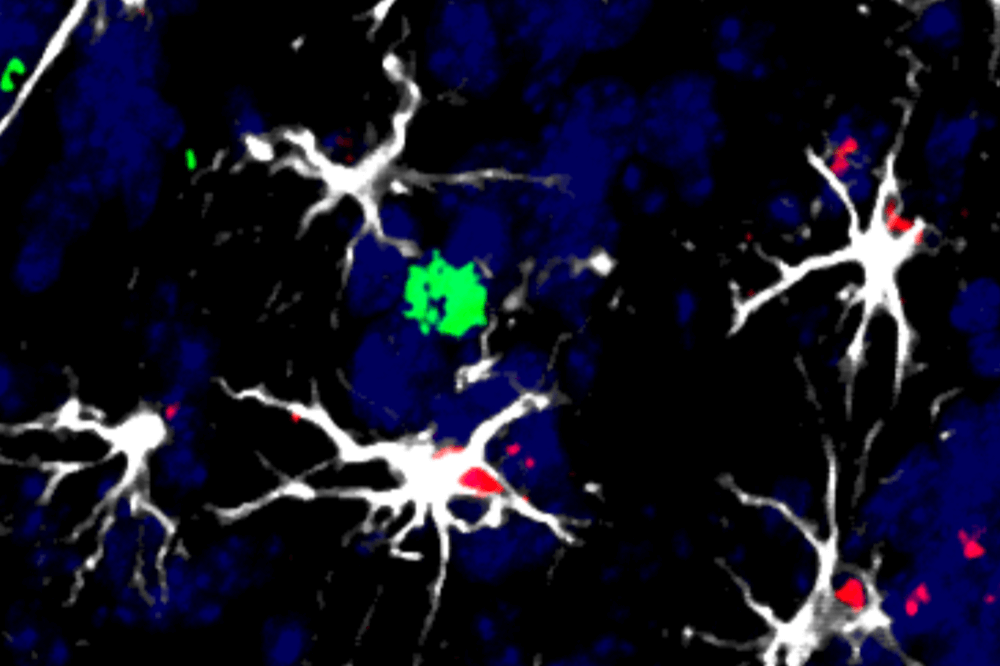
“We discovered -explains Nable Priego, The first signatory of the article is that a type of brain cell called astrocytes acts as immunomodulators, that is, they interact with the brain’s immune system, and in cases of brain metastasis, they abuse this function because they are influenced by the tumor. “.
Cancer-corrupted astrocytes side with tumor cells during brain metastases. The interaction of astrocytes with the immune system, which should be a normal process of immunomodulation, becomes a mechanism that feeds cancer, as astrocytes impede the work of protective cells and prevent them from killing tumor cells.
Biomarker of metastases for which immunotherapy will not work
The CNIO team identified a key molecule in this process called TIMP1. “Pro-tumor astrocytes produce TIMP1, and this protein is involved in turning off the protective cells that are supposed to kill cancer cells.”says Priego.
Once this molecule, TIMP1, has been shown to act on cells of the immune system and make them more ineffective, the CNIO team proposes using it as a biomarker to detect brain metastases that are affected by this mechanism of immunosuppression.
“TIMP1 is a good biomarker because in patients with brain metastases it is secreted into the cerebrospinal fluid in significantly higher quantities.”assures Priego.
A drug against protumor astrocytes is being tested
The research goes further. Manuel Valiente’s group proposes a therapeutic alternative targeting astrocytes: the combined use of immunotherapy with inhibitors that prevent the production of the TIMP1 molecule.
“There is a drug called silibinin, which is already being used for charitable purposes, that inhibits the production of the TIMP molecule.” Valiente notes. “Clinical trials are already underway to test its therapeutic efficacy in brain metastases. We hope to have results in 2025.”
The goal is to combine TIMP1 inhibition with traditional immunotherapy. “which will increase the effectiveness of the therapeutic strategy and facilitate its inclusion in clinical protocols”– says Brave.
Advancement in Basic Knowledge
This researcher also highlights another value of the work: identifying the role of astrocytes in disease. “unmasking their heterogeneity and attacking only those subtypes of astrocytes with altered and negative function for the patient.” “Until now, astrocytes have not been considered as immunomodulators, neither in general studies nor, of course, in relation to brain tumors. Our research is not only innovative from a clinical perspective, it is also very innovative for “advancing scientific research.” knowledge”emphasizes Valiente.
The work was funded by various national organizations such as the Spanish Association Against Cancer, the Ministry of Economy, Trade and Business (MINECO), the Carlos III Institute of Health, the La Caixa Foundation, the Ramón Areses Foundation or the Fundació. Marato TV3. It has also received funding from international organizations such as the European Research Council (ERC), the European Union through Next Generation Funds or the European Molecular Biology Organization (EMBO).
