shrinks in size in three out of seven colorectal cancer patients
Compilation
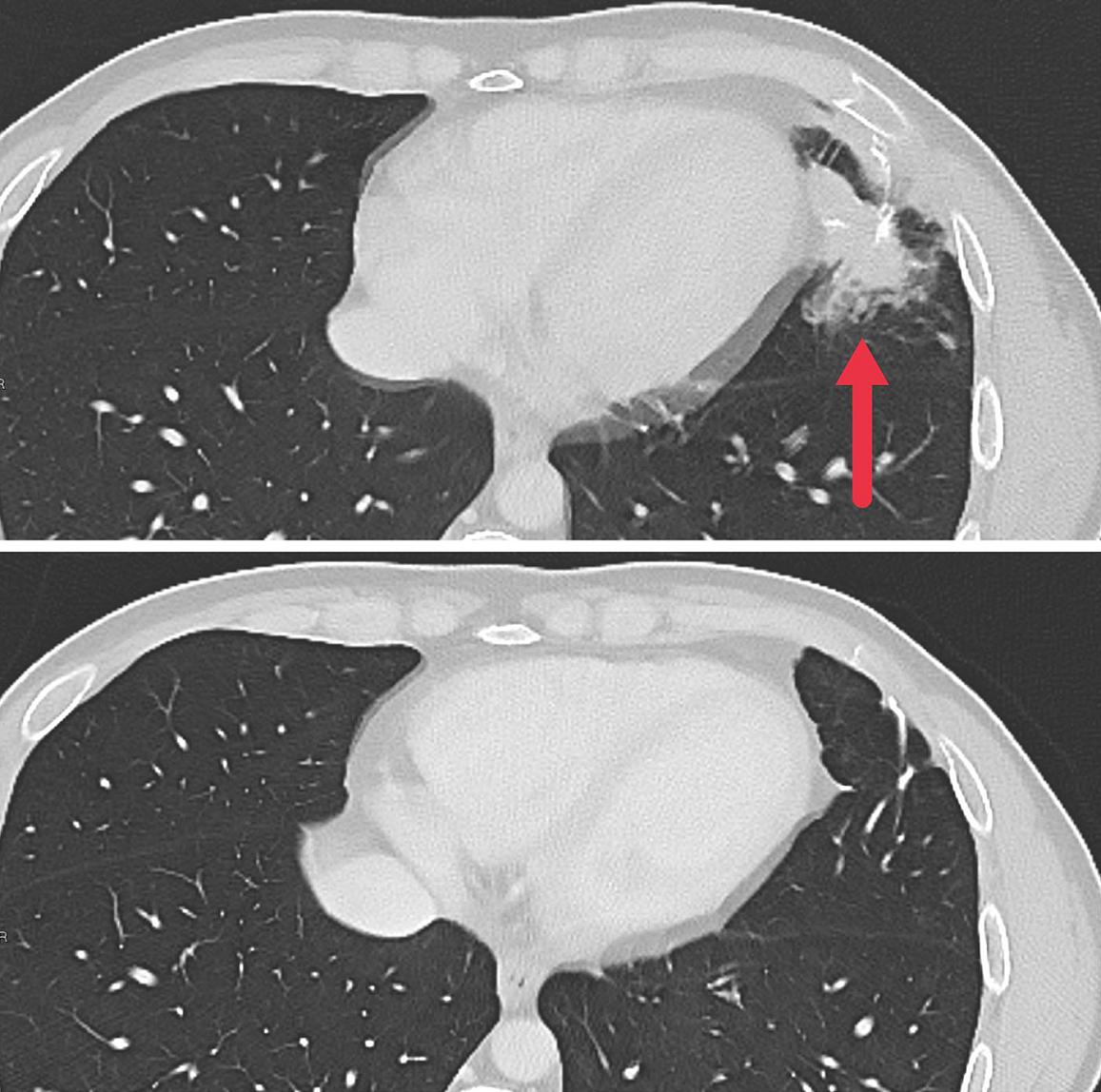
Initial results from clinical trials show that new strategy for cellular immunotherapy may be effective in the treatment of metastatic solid tumorsThis is evidenced by research published in the journal Nature Medicine and conducted by researchers from the National Institutes of Health (USA).National Institutes of Health of the United States) in the United States. The authors explain that They genetically modified each patient’s lymphocytes. so that they produced receptors that recognized and attacked their specific cancer cells. These initial results come from people with metastatic colorectal cancer who have already undergone several previous courses of treatment. Personalized immunotherapy reduced the size of tumors in several patients and This prevented them from growing back for up to seven months.
A form of cellular immunotherapy, T-cell therapy chimeric antigen receptors (CAR), has already shown its effectiveness against some types of blood cancer, and another, called tumor-infiltrating lymphocyte therapy (TIL), has proven effective against metastatic melanoma. However, There are currently no effective cell therapies against other solid cancers.according to Dr. Stephen A. Rosenbergfrom the NCI’s Center for Cancer Research (CCR), who led the study along with Dr. Maria Parkhurstfrom the CCR surgical service.


Dr. Rosenberg: “The ability to stop the growth of metastatic solid cancer shows that the new approach of cellular immunotherapy is promising”
«The fact that we can regression of metastatic solid cancer growth shows new approach to cellular immunotherapy promising. However, it is important to understand that these The results are preliminary and this approach needs to be refined and tested on more types. solid cancer— Rosenberg emphasized. New approach overcome two problems cellular immunotherapy: how to produce large quantities of T cells that can specifically recognize cancer cells, and how to enhance the ability of the modified T cells to proliferate once returned to the patient.
The researchers genetically modified each patient’s lymphocytes to produce receptors that recognized and attacked specific cancer cells.
For each patient in the study, Rosenberg and his team collected lymphocytes present in tumors patient. They then used complex molecular characterization methods identify and isolate receptors on these lymphocytes, called T-cell receptors, that recognize specific changes in each patient’s tumor. After genetically sequencing these receptors, they used a retrovirus to insert the receptor genes into normal lymphocytes collected from each patient’s circulating blood.
The genetically modified lymphocytes were expanded in the lab by the hundreds of millions and injected back into patients, where they expressed tumor-specific T-cell receptors and continued to proliferate.By taking natural T-cell receptors, which are present on very few cells, and introducing them into normal lymphocytes, of which we have a huge number, We can create as many cancer-fighting cells as we want.Yes— Rosenberg concluded.
