Stem cell transplant reverses diabetes and allows woman to produce insulin without injections
25 year old woman with type 1 diabetes became the first person in the world to restore insulin production after transplantation of pancreatic islets obtained from one’s own stem cells. This groundbreaking achievement from China could change the future of diabetes treatment, a disease that affects millions of people around the world.
Type 1 diabetes is a chronic disease in which the immune system attacks and destroys beta cells in the pancreas, which are responsible for producing insulin, a hormone needed to control blood glucose levels.
Until now, treatment options for these patients have been limited to daily insulin administration, with all the associated problems, including the risk of hypoglycemia and long-term complications.
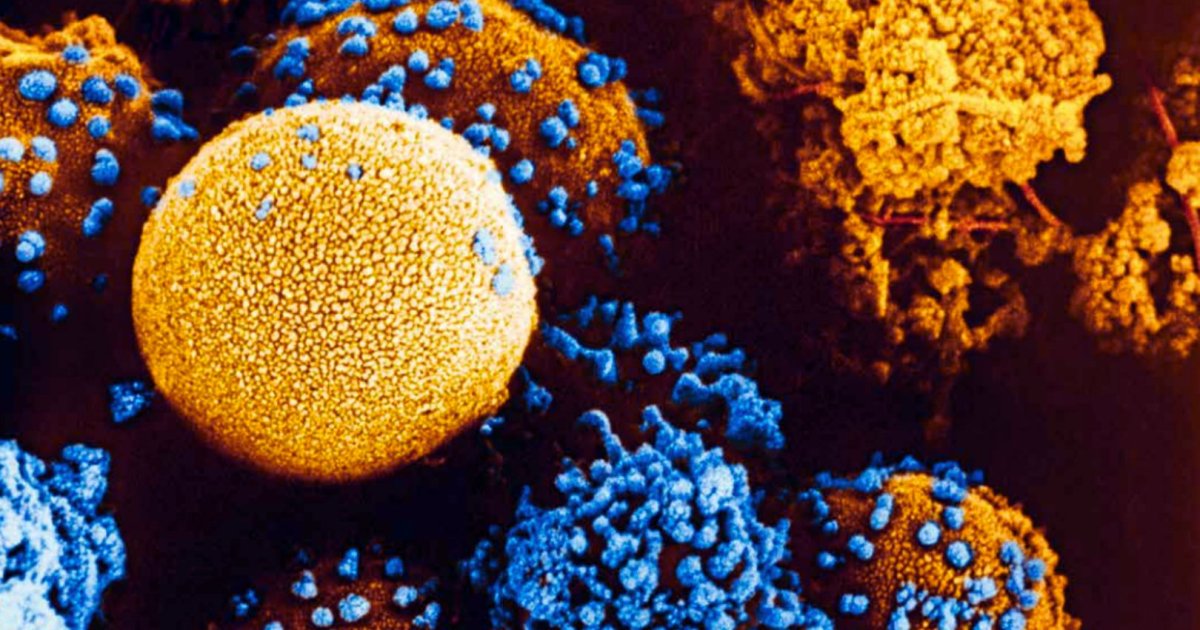
Scientists implanted reprogrammed pancreatic islets into the patient’s abdominal cavity, restoring insulin production. Photo: Istok / Christian Perez
New hope with reprogrammed stem cells
An innovative treatment that was announced just a few days ago in a journal. celldeveloped by a team of researchers led by Dr. Deng Hongkui from Peking University uses chemically induced pluripotent stem cells (ciPSCs) to create functional pancreatic islets. These stem cells are derived from the patient’s own somatic cells, eliminating the risk of immunological rejection and the need for immunosuppressive drugs, which often have significant side effects.
These types of stem cells are reprogrammed using small chemical molecules.in contrast to traditional methods that use genetic transcription factors. This approach provides greater control over the process and avoids genetic modification, a key advance in regenerative medicine.
In this case, The cells were obtained from the patient’s adipose tissue, reprogrammed and differentiated into pancreatic islets capable of producing insulin.. The islets were then transplanted under the sheath of the rectus abdominis muscle, a new site that allowed continuous monitoring by magnetic resonance imaging and the option of removing the cells in case of complications.
Pancreatic islets derived from stem cells began to produce insulin. This discovery could revolutionize the treatment of type 1 diabetes. Photo: Istok.
Surprising Results: Insulin Independence
Just two and a half months after transplantation, the patient began to produce insulin on her own, which allowed her to completely stop depending on exogenous insulin injections.. Over the course of a year, his insulin production stabilized and his glucose levels remained within the target range more than 98% of the time, an amazing achievement. In addition, their levels of glycosylated hemoglobin, a measure of long-term glucose control, remained within normal limits.
Just two and a half months after the transplant, the patient began to produce insulin on her own.
The patient, who had previously struggled to maintain adequate control of her diabetes despite a strict insulin regimen, described these changes as transformative. “Now I can eat sugar,” he commented in a telephone conversation with the prestigious magazine. Nature. To which he also noted that “I like to eat everything, especially stew.”
This success not only marks remarkable progress for this particular patient, but also opens the door to potential new treatments for millions of people with type 1 diabetes around the world. According to Dr. James Shapiro, an expert in islet transplantation and diabetes at the University of Alberta, “The results are exciting. “They completely reversed diabetes in this patient, who previously required large amounts of insulin.”
The future of type 1 diabetes treatment
The Chinese study is part of a growing number of pioneering clinical trials aimed at treating diabetes using stem cells. Although donor-derived pancreatic islet transplantation has been used in the past with some success, the lack of suitable donors and the risks associated with the use of immunosuppressive drugs have limited the expansion of this therapy.
On the other hand, stem cells offer a potentially unlimited supply of pancreatic islets. Most importantly, by using patient-derived cells, the need to suppress the immune system is eliminated, which can significantly reduce long-term risks.
The first patient with type 1 diabetes to produce insulin again thanks to a transplant of pancreatic islets derived from her own stem cells. Photo: Istok
Despite the impressive results in this first case, the researchers note that more research is needed to confirm the treatment’s effectiveness in other patients. Dr. Deng’s team has already treated two other participants whose evaluations also showed positive results. A further 10-20 people are expected to take part in the trial in the coming months.
Problems and next steps
One of the biggest challenges in scaling up this type of treatment is the cost and complexity of the process. Creating islets from a patient’s own cells requires advanced technology and considerable time, making it difficult to implement on a large scale.
However, pharmaceutical companies such as Vertex Pharmaceuticals are also exploring the possibility of using donated stem cells to create islets that can be used in more patients.
3D illustration of a molecule of the human hormone insulin. Photo: Istok
In the meantime, scientists continue to work to improve the safety and effectiveness of stem cell-derived islet transplants. One long-term goal is to create islets that are not attacked by the immune system of patients with type 1 diabetes.eliminating the need for any type of immunosuppression. If achieved, this achievement could mean a real cure for a disease that until now could only be controlled.
As we see it, this transplant marks an important milestone in regenerative medicine and brings new hope to millions of people around the world living with type 1 diabetes. Although there is still some way to go before this treatment becomes widely available, early results are promising. and could change the way this disease is treated forever.
Links:
- Wang S, Du Y, Zhang B, et al. Transplantation of chemically induced pluripotent stem cell-derived islets under the anterior rectus sheath in a patient with type 1 diabetes. cell. Published online September 20, 2024. doi:10.1016/j.cell.2024.09.004.
- Mallapati S. Stem cells reverse female diabetes – a world first. Nature. Published online September 26, 2024. doi:10.1038/d41586-024-03129-3.

