They found a link between abdominal fat and signs of Alzheimer’s disease 20 years before the onset of symptoms.

A recent scientific study found connection a very important thing that happens in our body between obesity, abdominal fat distribution and risk the disease will develop early Alzheimer’s disease.
Research presented at the annual meeting Radiological Society of North America (RSNA) in 2024 showed how excess visceral fataccumulated deep in the stomach, This is associated with increased levels of beta-amyloid and tau proteins.both early markers of Alzheimer’s disease.
This discovery, made in cognitively healthy middle-aged people, may be a fundamental clue to prevent disease decades before cognitive symptoms appear.
Physician-led study Mahsa Dolatshahi and Cyrus A. Raji, was conducted with 80 participants aged 40 to 50 years. Approximately 57.5% of the participants were obese, and the average body mass index (BMI) of the participants was 32.31, which is considered obese.
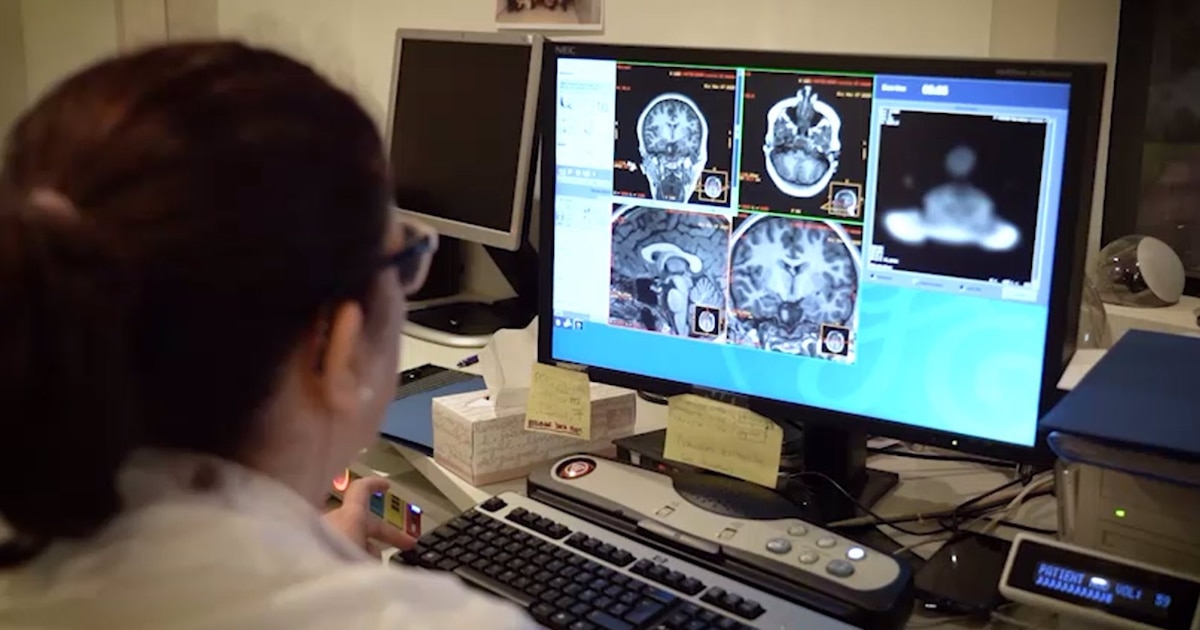
Candidates passed brain positron emission tomography (PET), body MRI and metabolic assessment (glucose and insulin measurements), and a lipid (cholesterol) panel. An abdominal MRI was performed to measure the volume of subcutaneous fat (fat under the skin) and visceral fat (deeply hidden fat surrounding the organs).

In the study, the researchers focused on how visceral fat, a form of deep fat that surrounds internal organs, affects the brain, especially the brain. deposition of abnormal proteins associated with Alzheimer’s disease.
Experts indicated that Visceral fat is more metabolically active than subcutaneous fat, which is located under the skin. According to research, this type of fat not only promotes inflammation in the body, but also directly affects the brain. “The more visceral fat a person has, the more inflammation occurs in the body, and it’s actually much worse than the inflammation caused by subcutaneous fat,” Raji explained.
Using magnetic resonance imaging (MRI) and positron emission tomography (PET), researchers were able to observe that high levels of visceral fat correlated with increased protein content. Beta-amyloid and tau in the brains of participants before symptoms of Alzheimer’s disease became apparent. These proteins are known to form plaques and tangles in the brains of Alzheimer’s patients, disrupting communication between brain cells and contributing to cognitive decline.
“What’s new is that we show for the first time that more visceral fat is associated with abnormally high levels of tau protein in people 20 years before they may develop the first symptoms of Alzheimer’s disease,” Raji said. Thus, this finding highlights the importance of monitoring visceral fat as a key factor in preventing neurodegenerative diseases.

The discovery adds to growing global concern about obesity, which affects more than 40% of adults in many developed countries. According to World Health Organization (WHO), obesity has reached epidemic levels, which increases the risk of developing various chronic diseases, including dementia. In this context, research shows how the accumulation of visceral fat even in early middle age can trigger a pathological process that, if left unchecked, can lead to the manifestation of Alzheimer’s disease many years later.
The study also found that people with more visceral fat had increased risk of brain atrophy, another important biomarker of Alzheimer’s disease.
Brain atrophy is the loss of brain mass, a process associated with shrinkage of the hippocampus, the area of the brain responsible for memory.
In addition, the researchers emphasized that Obesity not only affects the brain, but also blood circulation. A previous study presented at the same conference noted that visceral fat can reduce cerebral blood flow, further impacting cognitive health.

The fact that obesity, and especially visceral fat, is associated with these early changes in the brain calls for new strategies for preventing Alzheimer’s disease.
Researcher Mahsa Dolatshahi emphasized that the study suggests that lifestyle changessuch as weight loss and reduction in visceral fat may be fundamental to prevent or at least delay the onset of the disease.
“This is a discovery opens the door to new treatment optionsboth through lifestyle changes and possible pharmacological interventions to reduce abdominal fat,” Dolatshahi said. In this sense, promoting healthy habits, such as a balanced diet and regular exercise, appears to be a key tool in combating visceral obesity and its consequences on the brain.
The study also highlights the importance eliminate metabolic factors associated with obesity, such as insulin resistance and cholesterol levels, which, according to the results, also have a direct effect on the accumulation of amyloid and tau proteins.

The discovery of this link between visceral fat and Alzheimer’s disease is particularly relevant in the context of global public health. With the world’s population aging and a growing number of people at risk of developing dementia, researchers warn of an urgent need for action to combat obesity and the accumulation of visceral fat.
“We’re trying to understand why obesity in midlife, between ages 40 and 50, is a risk factor for Alzheimer’s disease, which typically doesn’t become symptomatic until age 60, 70 or 80,” Raji explained. Early intervention in midlife may be critical to reducing the risk of Alzheimer’s disease in future generations.
Additionally, experts note that while obesity and visceral fat accumulation are known risk factors, longer-term studies are needed to better understand how these conditions lead to cognitive decline. Advances in imaging techniques such as PET and MRI scanners are promising tools. identify these pathological changes in the early stages and perhaps before the development of the most obvious symptoms.

Despite the complexity of the study and its implications, the researchers also emphasize that reducing the amount of visceral fat is possible through lifestyle changes. Moderate exercise and a healthy diet are two basic principles in the fight against abdominal obesity.
Preventive neurologist Richard Isaacsonwho was not directly involved in the study, noted that “we should focus not only on body weight, but also on body composition.”
Exercises in fat burning zones and strength training These are strategies that can improve metabolic health and reduce visceral fat over the long term, which can positively impact brain health.
Thus, the study not only highlights an important scientific finding, but also highlights the importance of early intervention in midlife to prevent Alzheimer’s disease, offering new perspectives for addressing this growing public health problem.
